What to Know
- Priscilla Chan and her husband, Facebook founder Mark Zuckerberg, funded one of California's first large-scale COVID-19 testing labs, providing free testing to counties around the state
- The lab at the Chan-Zuckerberg Biohub in San Francisco analyzed the genetics of virus samples from across California to learn how the coronavirus spreads, and also processed test results for an intensive study in San Francisco's Mission District
- The study revealed startling realities about the disproportionate effects of the virus on the Latino community, and the barriers that need to be overcome to keep that community safe
On a windy January afternoon, a line of people snaked its way around the corner of 24th and Mission in San Francisco, meandering around street vendors and shop entrances in the heart of a bustling neighborhood.
Wearing masks and occasionally face shields, the people in line dutifully stood on chalked lines six feet apart, each waiting their turn to have their nostrils probed by a stranger holding an extra-long cotton swab.

"For the first few days, we had over 700 people (per day) come test," said Susana Rojas, executive director of Calle 24, San Francisco's Latino Cultural District.
First opened in April 2020 for a select group of residents, the free coronavirus testing site at the corner of 24th and Mission had been open to all members of the public since November, and after a holiday surge in COVID-19 cases, it saw no shortage of takers.
"It was huge," Rojas said of the surge when we spoke in January. "And we're hoping that with all the work we're doing to help people isolate, we're going to be able to bring it down."

Helping infected people stay isolated, explained UCSF physician Carina Marquez, is key to stopping the spread — and in this predominantly Latino neighborhood, that comes with unique challenges. The first challenge, she said, is simply catching the infection before it spreads to an entire family.
Local
Get a weekly recap of the latest San Francisco Bay Area housing news. >Sign up for NBC Bay Area’s Housing Deconstructed newsletter.
"Transmission within households is really high, and certainly higher when you're exposed to more people," she said. "Especially in really dense households, where you're living with your grandma and your aunts and uncles and there's lots of kids."
A New Approach From an Old Playbook
Marquez and her collaborator Diane Havlir at UCSF saw striking similarities between this pandemic and the one that raged out of control in the Bay Area a generation ago: the HIV/AIDS pandemic. Though the two viruses are very different in how they work and spread, they believed an effective response to the coronavirus could take a page straight out of Havlir's HIV playbook from the 1980s.
"We developed an approach we call 'low barrier,'" Havlir said. "A person can walk up on that same very day, they can get the result as soon as possible, and they can have someone help navigate what they should do with that result."

Those principles formed the basis of the Mission District community testing site when it first opened to a select group of study participants in April, 2020. Testing was free, with no need to show an ID or insurance card, and no appointment necessary. Those eligible were encouraged to test often — at the first sign of symptoms, or with no symptoms at all. Results were delivered the same day by a disclosure team that could immediately offer counseling and services to patients who tested positive.
It was a highly unusual approach in the early days of the pandemic, recalled UCSF biophysics professor Joe DeRisi.
"A year ago, to qualify to get a test you had to be symptomatic," DeRisi said. "That was a major, major mistake."
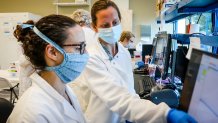
DeRisi set up one of California's first large-scale coronavirus testing labs in San Francisco, funded by Priscilla Chan and Mark Zuckerberg and housed at the Chan Zuckerberg Biohub, where DeRisi serves as co-president.

"We just didn't fully appreciate that around 50 percent of people who get COVID never have a symptom," he said. "And that one fact is probably the largest driver of this pandemic, bar none."
Processing test samples from around the state — and from the Mission District study — he began analyzing tiny mutations in the virus to build a "family tree" of sorts, and learn about how it spreads. The analysis showed that essential workers are some of the most likely people to contract the virus, and densely-packed living situations are the places where it spreads the fastest. As Havlir's study gathered more information about the demographics of those who tested positive, a troubling pattern began to emerge.
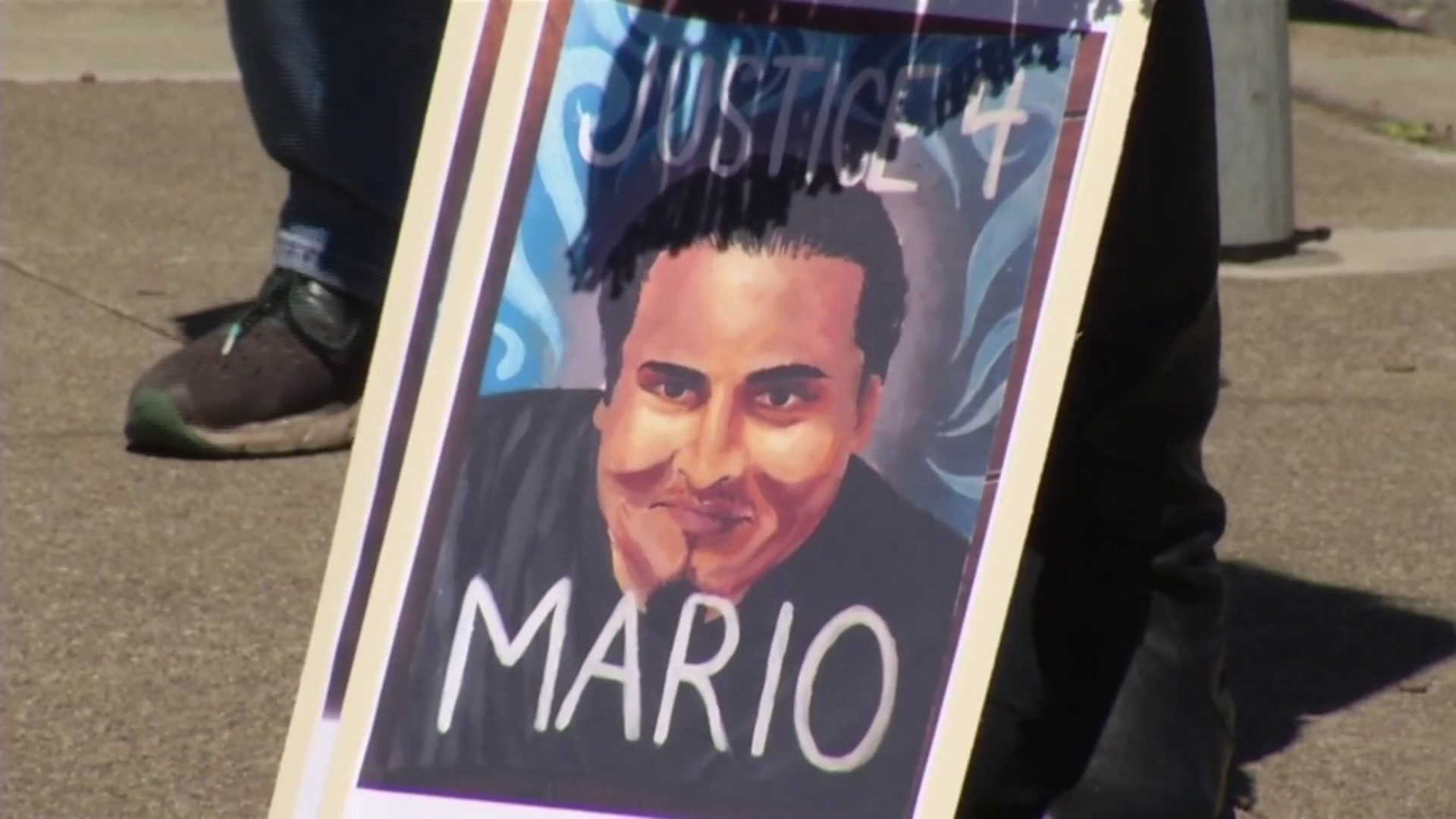
A Community Hit Hard
According to the Latino Task Force, which partnered with UCSF on the study, about 40 percent of the people tested in the study identified themselves as Latino (Latinos make up 58 percent of the neighborhood overall). But among people who tested positive for COVID-19, Latinos account for a staggering 95.5 percent.
"I wasn't surprised — but I was devastated," Priscilla Chan said of her first look at those numbers. "The number of people who identified as Caucasian with coronavirus, I think, was literally zero. Zero. In the same neighborhood, in the same buildings."
Chan oversees the day-to-day operations of the Chan Zuckerberg Initiative, the philanthropy she runs with her husband, Facebook founder Mark Zuckerberg. The organization's stated goal is to cure, prevent or manage all disease by the end of the century. Chan has strong feelings about inclusivity when it comes to health care: in public health, she says, the "public" must include everybody.
"The Latinx population that traditionally has lower access to healthcare and testing needs a different solution," she said. "To keep everyone safe, we actually have to keep everyone safe."
The Chan Zuckerberg Initiative initially pledged $13.6 million to study the spread of COVID-19 in the Bay Area, and as of April 2021, had spent a total of $108.8 million on coronavirus response efforts worldwide. $4.7 million of that went to set up and run the testing lab overseen by DeRisi, which provided free PCR testing to counties across California.

But for the Latino community in San Francisco's Mission District, traditional approaches to PCR testing often weren't fast enough.
"Waiting two days, three days, sometimes five days to get your result," Marquez said, "by the time we get to the home, everybody's been infected."
So in the fall of 2020, the UCSF team began trying out a new kind of test at the Mission community site: Abbott's BinaxNOW rapid antigen test, which comes on a paper card and requires no machine or special processing. The test gives a result within 15 minutes, meaning volunteers can notify patients within 1-2 hours. By January, the site had switched to the new test entirely, with thousands of data points confirming that it was nearly as accurate as PCR at identifying the patients with the highest viral loads — those most likely to be infectious.

"Identifying people earlier on in their infection may mean that you can get to their contacts a lot earlier," Marquez said.
She explained that COVID-19 is typically contagious for ten days from the onset of symptoms. Patients who drop by for testing at the first sign of a fever could be notified of their need to isolate on the first day — meaning they can avoid spreading the virus for the remaining nine days. That stands in stark contrast to PCR testing by appointment, in which a patient could unknowingly spread the virus for several days — while waiting for a test, and then waiting for a result.
A Problem of Economics
The importance of a rapid test-and-respond model is only amplified by the economic realities facing the Latino community in San Francisco's Mission District, said Jon Jacobo of the Latino Task Force.
"It's highlighting these inequities within our country," said Jacobo, who chairs the task force's health committee.
Compounding the problem of crowded apartments, Jacobo said, is the list of jobs most commonly held by Latinos in San Francisco: jobs that are high-risk for coming in contact with people carrying the coronavirus.
"Ask yourself: who's picking the food in the fields?" he said. "Who's driving the trucks to the produce market? Bringing it to the grocery stores? Taking it to the restaurants? ... It's the Latino community."

Of the people who tested positive during the initial study, he said, "We found that 90 percent of them were essential workers — meaning they couldn't stay home, they had to go out and work. And 88 percent of them made under $50,000 a year — in a neighborhood where a two-bedroom goes for $4,500 a month. That leads to people having to live multiple individuals in a unit."
In San Francisco, it's common for landlords to ask that prospective tenants prove they're spending no more than a third of their income on rent — meaning that it would take three incomes at those wages to qualify for a lease on a two-bedroom apartment.
Because people working in those types of jobs may have multiple employers and irregular hours, the ability to get tested in their own neighborhood without a prior appointment was a major step toward making testing more accessible, Havlir said. Marquez added that self-isolation in a large household is often a tricky matter. Breaking down that barrier came with help from San Francisco's public health department.

"The Department of Public Health offers a free hotel, and so we immediately — same day you get diagnosed — we can refer you to ... stay in a free hotel during your isolation period, with the hope that you're going to decrease the likelihood that you spread the infection to your roommates," Marquez said. "And then, of course, we want the roommates to come here and test."
For households of more than four people, the disclosure team will offer to make a house call: they'll come to the patient's home, test everyone who lives there, and immediately offer services that could include food assistance if the need to isolate will result in lost wages.
"It's not enough to test," Marquez emphasized. "You have to respond."
A Summer of Uncertainty
Even with all adults now eligible for vaccines across much of the Bay Area, DeRisi says testing will remain important.
"There's still a sizable percentage of the population that isn't vaccinated yet," he said. "We need to know who has the virus, and we need to isolate them quickly — especially with the emergence of new variants."

DeRisi's genetic testing lab continues to analyze samples from around the state — looking for which variants are entering the Bay Area, which are becoming dominant, and which could spell trouble.
"We want to know if there are particular variants that not only spread aggressively, but might have the ability to escape the vaccine," he said.
UCSF and the Latino Task Force are continuing to offer community testing, and Jacobo said the 24th and Mission site has been responsible for about six percent of the samples sent in for genetic sequencing.
The site has also begun offering vaccinations, inviting those who get tested to book a vaccine appointment before leaving — and sending out invitations by text message to those who've been tested there in the past. Havlir points out that some of the obstacles that exist at large city-run testing sites can also exist at mass vaccination sites.
"There's people that there are just trust barriers, cultural barriers, to go to large sites like that, and those are the people we need to offer vaccination opportunities to," Havlir said.
A Group That's Still Waiting
But as more people get vaccines, there's one group that's remained almost completely unvaccinated: children. DeRisi and Chan point out that testing is likely to play a critical role in safely reopening schools.
As the mother of two school-age daughters, Chan said she knows this year has been tough on kids.
"One thing that is critical is making sure that our kids are getting back to their 'normal,' whatever the new normal is," she said. "They need to be with other kids, they need to be learning."
And though the Chan Zuckerberg Initiative's long term focus on supporting breakthroughs in basic science remains the same, Chan said she's taking a hard look at how the organization can continue some of the work it's begun during this unexpected detour.
Above all, Chan said, she hopes the pandemic has highlighted that the public health of a community is only as strong as its most vulnerable population.
"To actually address the pandemic, we have to act as a collective body, and that doesn't work if we're systematically leaving populations behind," she said. "We get sick together; we get well together."