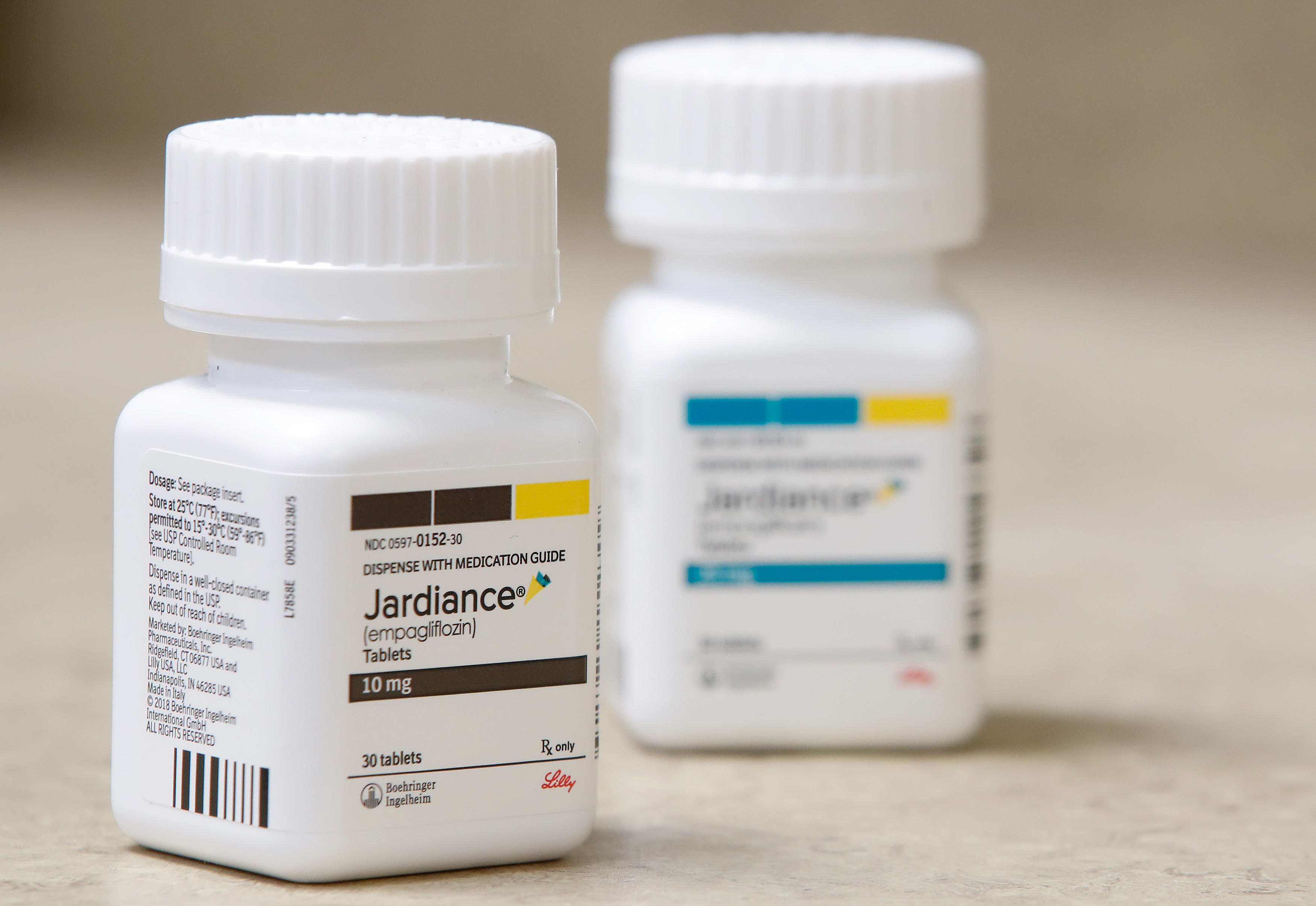
The popular diabetes treatment Jardiance and the blood thinner Eliquis are among the first drugs that will be targeted for price negotiations in effort to cut Medicare costs.
President Joe Biden's administration on Tuesday released a list of 10 drugs for which the federal government will take a first-ever step: negotiating drug prices directly with the manufacturer.
The move is expected to cut costs for some patients, but faces litigation from the drugmakers and heavy criticism from Republican lawmakers, and it will be years before consumers notice any savings.
The effort is a centerpiece of Biden's reelection pitch as the Democrat seeks to show Americans he's deserving of a second term because of the work he's doing to lower costs for them while the country is struggling with inflation. But like the drug negotiations, many of Biden's biggest policy moves take time to roll out, and his challenge is to persuade the public to be patient.
“For many Americans, the cost of one drug is the difference between life and death, dignity and dependence, hope and fear,” Biden said in a statement. “That is why we will continue the fight to lower healthcare costs — and we will not stop until we finish the job.”
The drugs on the list announced Tuesday accounted for more than $50 billion in Medicare prescription drug costs between June 1, 2022, and May 31, according to the Centers for Medicare and Medicaid Services, or CMS.
That includes more than $16 billion on Eliquis. The drug from Pfizer and Bristol-Myers Squibb treats blood clots in the legs and lungs and reduces the risk of stroke in people with an irregular heartbeat called atrial fibrillation.
Senior administration officials said Tuesday that the 10 drugs selected for negotiation are among the most costly to the Medicare program. They said 8.2 million people with Medicare Part D prescription drug coverage take them.
The diabetes treatments Jardiance from Eli Lilly and Co. and Boehringer Ingelheim and Januvia from Merck made the list. It also included Amgen’s autoimmune disease treatment Enbrel and Entresto from Novartis, which is used to treat heart failure.
Get a weekly recap of the latest San Francisco Bay Area housing news. >Sign up for NBC Bay Area’s Housing Deconstructed newsletter.
Other drugs on the list include AstraZeneca’s diabetes and heart failure treatment Farxiga and three drugs from Johnson & Johnson: the blood thinner Xarelto, the blood cancer treatment Imbruvica and it’s biggest seller, Stelara, an IV treatment for psoriasis and other inflammatory disorders.
The list also includes several versions of Novo Nordisk’s Fiasp, a fast-acting insulin taken around meals.
| Drug Name | Commonly Treated Conditions | Total Part D Gross Covered Prescription Drug Costs from June 2022-May 2023 | Number of Medicare Part D Enrollees Who Used the Drug from June 2022-May 2023 | Average Part D Covered Prescription Drug Costs Per Enrollee |
| Eliquis | Prevention and treatment of blood clots | $16,482,621,000 | 3,706,000 | $4,448 |
| Jardiance | Diabetes; Heart failure | $7,057,707,000 | 1,573,000 | $4,487 |
| Xarelto | Prevention and treatment of blood clots; Reduction of risk for patients with coronary or peripheral artery disease | $6,031,393,000 | 1,337,000 | $4,511 |
| Januvia | Diabetes | $4,087,081,000 | 869,000 | $4,703 |
| Farxiga | Diabetes; Heart failure; Chronic kidney disease | $3,268,329,000 | 799,000 | $4,091 |
| Entresto | Heart failure | $2,884,877,000 | 587,000 | $4,915 |
| Enbrel | Rheumatoid arthritis; Psoriasis; Psoriatic arthritis | $2,791,105,000 | 48,000 | $58,148 |
| Imbruvica | Blood cancers | $2,663,560,000 | 20,000 | $133,178 |
| Stelara | Psoriasis; Psoriatic arthritis; Crohn's disease; Ulcerative colitis | $2,638,929,000 | 22,000 | $119,951 |
| Fiasp; Fiasp FlexTouch; Fiasp PenFill; NovoLog; NovoLog FlexPen; NovoLog PenFill | Diabetes | $2,576,586,000 | 777,000 | $3,316 |
The Inflation Reduction Act already caps Medicare patient out-of-pocket costs for insulin at $35 a month. An administration official said Tuesday that upper limit will hold but there could be further changes in those costs.
The announcement Tuesday is another significant step toward taming drug pricing under the Inflation Reduction Act, which was signed by Biden last year. The law also calls for a $2,000 annual cap on how much people with Medicare have to pay out of pocket for drugs starting in 2025.
For drugs on the list released Tuesday, the government aims to negotiate the lowest maximum fair price. That could help some patients who have coverage but still face big bills like coinsurance payments when they get a prescription.
About 9% of Medicare beneficiaries age 65 and older said in 2021 that they did not fill a prescription or skipped a drug dose due to cost, according to research by the Commonwealth Fund, which studies health care issues.
Health Secretary Xavier Becerra said earlier this year that the drugs would be selected from a list of the 50 most expensive for Medicare Part D. The selection process included the drug having been on the market for at least seven years without generic competition, or 11 years in the case of biological products such as vaccines, CNBC reports.
HHS will make its initial offer to the pharmaceutical companies in February 2024. The companies will have 30 days to accept the offer or propose a counter offer.
The negotiations will end in August 2024, and HHS will publish the agreed upon costs in September. The negotiated prices for those 10 Medicare Part D drugs will go into effect in January 2026.
Drug companies that refuse to be a part of the new negotiation process will be heavily taxed.
Another 15 Medicare Part D drugs are expected to be up for negotiation in the program's second phase, with prices taking effect in 2027.
Currently, pharmacy benefit managers that run Medicare prescription plans negotiate rebates off a drug's price. Those rebates sometimes help reduce premiums customers pay for coverage. But they may not change what a patient spends at the pharmacy counter.
The new drug price negotiations aim "to basically make drugs more affordable while also still allowing for profits to be made,” said Gretchen Jacobson, who researches Medicare issues at Commonwealth.
The pharmaceutical industry has been gearing up for months to fight these rules. Already, the plan faces several lawsuits, including
The federal government will benefit most from any lowered drug prices, noted Larry Levitt, an executive vice president for health policy at KFF, another non-profit that studies health care. But he said that if Medicare spends less on prescription drugs, then premiums for everyone with its drug coverage also should fall.
Drug companies that refuse to be a part of the new negotiation process will be heavily taxed.
The pharmaceutical industry has been gearing up for months to fight these rules. The lobbying group Pharmaceutical Research and Manufacturers of America said Tuesday that the drug list announcement stemmed from “a rushed process focused on short-term political gain rather than what is best for patients.”
“Many of the medicines selected for price setting already have significant rebates and discounts due to the robust private market negotiation that occurs in the Part D program today,” PhRMA CEO Stephen J. Ubl said in a statement.
PhRMA representatives also have said pharmacy benefit managers can still restrict access to drugs with negotiated prices by moving the drugs to a tier of their formulary — a list of covered drugs — that would require higher out-of-pocket payments. Pharmacy benefit managers also could require patients to try other drugs first or seek approval before a prescription can be covered.
PhRMA and several drugmakers have filed lawsuits over the administration's plan.
The federal government will benefit most from any lowered drug prices, noted Larry Levitt, an executive vice president for health policy at KFF, another non-profit that studies health care. But he said that if Medicare spends less on prescription drugs, then premiums for everyone with its drug coverage also should fall.
Drug companies that refuse to be a part of the new negotiation process will be heavily taxed.
The pharmaceutical industry has been gearing up for months to fight these rules. The lobbying group Pharmaceutical Research and Manufacturers of America said Tuesday that the drug list announcement stemmed from “a rushed process focused on short-term political gain rather than what is best for patients.”
“Many of the medicines selected for price setting already have significant rebates and discounts due to the robust private market negotiation that occurs in the Part D program today,” PhRMA CEO Stephen J. Ubl said in a statement.
PhRMA representatives also have said pharmacy benefit managers can still restrict access to drugs with negotiated prices by moving the drugs to a tier of their formulary — a list of covered drugs — that would require higher out-of-pocket payments. Pharmacy benefit managers also could require patients to try other drugs first or seek approval before a prescription can be covered.
PhRMA and several drugmakers have filed lawsuits over the administration's plan.
Republican lawmakers also have blasted the Biden administration, saying companies might pull back on introducing new drugs that could be subjected to future haggling. They’ve also questioned whether the government knows enough to suggest prices for drugs.
___
Murphy reported from Indianapolis.